- Have any questions? Contact us!
- info@dr-rath-foundation.org

Our Study Proves That Heart Disease Is Linked To Vitamin C Deficiency
October 4, 2017
The Benefits of Micronutrients for Healthy Eyes
October 4, 2017Heart disease confirmed as an early form of scurvy
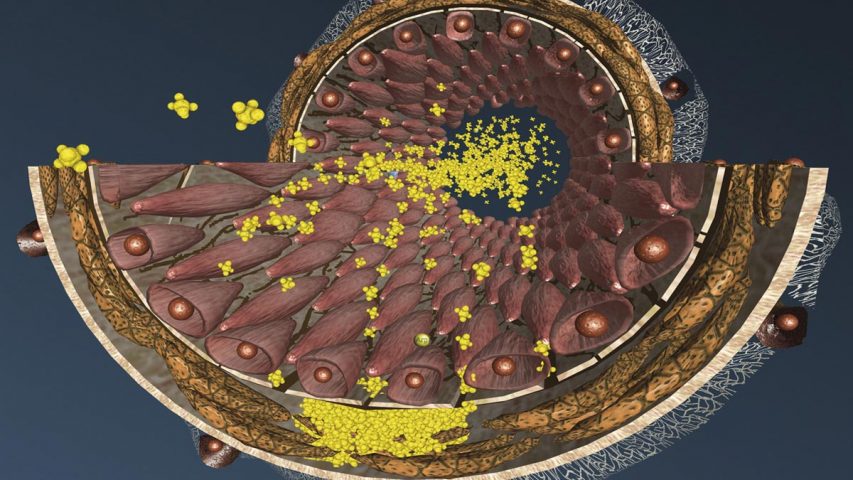
Atherosclerosis is mainly a result of chronic vitamin deficiency in our diet. The hallmark of early atherosclerosis is the structural weakness of the arterial wall, characterised for example by the gaps between the endothelial cells (see fig.). As a result, there are deposits of repair molecules which finally cause the feared atherosclerotic plaques.
Scurvy (also known as the “Sailors’ Disease”) is a condition resulting from a complete bodily depletion of ascorbic acid (vitamin C). It is a fatal disease characterized by a slow dissolution of connective tissue throughout the body, including the walls of the blood vessels. This disease was quite common in earlier centuries, especially among sailors whose diets were deprived of vitamin C. During long voyages at sea many sailors died within months from tremendous blood loss. Today, fully developed scurvy is rare; however, subclinical scurvy is very common especially in the elderly, infants, children on special diets and people with poor dietary habits.
Vitamin C is essential for the production of collagen and other connective tissue components in the body. Most animals synthesize their own vitamin C according to needs. However, about 40 million years ago this ability was lost in our human ancestors as a result of a genetic mutation. Therefore, we have to obtain vitamin C from our diet or through nutritional supplements.
Dr. Rath introduced the groundbreaking concept of a “Scurvy-vitamin C-heart disease connection” over two decades ago. According to this concept heart disease is an early form of scurvy, a condition that increases the need for biological repair of weakened arterial walls due to impaired collagen synthesis in the body. As a consequence, cholesterol transporting molecules such as LDL and Lp(a) deposit in the vascular walls as reinforcing factors, but, at the same time, contribute to a buildup of atherosclerotic plaques and increase the risk of heart attack or stroke.
The connection between vitamin C and atherosclerosis was confirmed in a scientific experiment in guinea pigs that, similar to humans, cannot produce their own vitamin C1. We observed that guinea pigs fed a five-week diet deprived of vitamin C developed atherosclerotic deposits in the arterial tree, accompanied by damage to the inner lining of the artery wall, specifically in areas closer to the heart at the site of maximum mechanical stress. However, animals supplemented with vitamin C did not show any significant structural changes in their blood vessels. This study confirmed that the invariable consequence of ascorbate deficiency is a loosening of the connective tissue and loss of the protective barrier in artery walls.
Another important feature of human metabolism is its ability to produce a specific lipoprotein – lipoprotein(a) – which is absent in animal species. Dr. Rath proposed that the appearance of Lp(a) at the time of the loss of vitamin C production had offered a significant advantage to the ancestors of man2. The Lp(a) can act as a physiological surrogate to compensate for vitamin C deficiency by protecting the integrity of blood vessel walls. In order to avoid the fatal consequences of extreme ascorbate depletion, such as hemorrhagic bleeding, our body increases the concentration of specific “repair” factors including Lp(a) and fibrinogen etc. These temporary “repair” factors can compensate for the connective tissue impairment, but if vitamin C insufficiency continues the repair process overshoots resulting in atherosclerotic build up and leading to heart attacks and strokes.
Recently, we confirmed the vitamin C – Lp(a) – heart disease connection3 using our unique animal model which mimics human metabolism in respect to its two critical aspects: inability to synthesize vitamin C (Gulo-/-) and internal synthesis of human Lp(a) (Lp(a)+). We observed that {Gulo-/-;Lp(a)+} mice fed a diet low in vitamin C have a high level of Lp(a) deposits in the vascular walls, develop atherosclerotic plaques and have increased blood levels of Lp(a) compared to animals supplemented with high doses of vitamin C.
While our study confirms that vitamin C is essential to maintain healthy blood vessels and reduce atherosclerosis, the Dr. Rath Research Institute has also clinically proven that vitamin C is not the only nutrient that is critical in maintaining a healthy cardiovascular system. We have established that vitamin C, in combination with the amino acids lysine, proline and other specific nutrients, is vital for maintaining healthy arteries and the cardiovascular system.
Ref:
1 M. Rath, L. Pauling, Proc. Nati. Acad. Sci. USA Vol. 87, pp. 6204-6207, 1990
2 M. Rath, L. Pauling; Journal of Orthomolecular Medicine 1991, 6:125-134
3 J. Cha, A. Niedzwiecki, M. Rath; Am J Cardiovasc Dis 2015;5(1):53-62



