- Have any questions? Contact us!
- info@dr-rath-foundation.org

Higher Omega-3 Levels Linked To Less Depression In Heart Failure Patients
August 29, 2018
Study Portrays Dangerous Weight-Loss Drug As Safe And Effective
August 30, 2018How To Prevent And Control Osteoporosis Naturally, Without Drugs
Osteoporosis is the world’s most common chronic bone disease. Characterized by increased bone fragility, it is seen in all age groups, genders, and races. It is estimated that more than 200 million people globally suffer from this disorder. Statistics from the International Osteoporosis Foundation suggest that 1 in 3 women over the age of 50 years and 1 in 5 men will experience osteoporotic fractures during their lifetime. Fortunately, therefore, Dr. Rath’s Cellular Medicine approach now provides the possibility to prevent and control the osteoporosis epidemic naturally, without drugs.
What is osteoporosis?
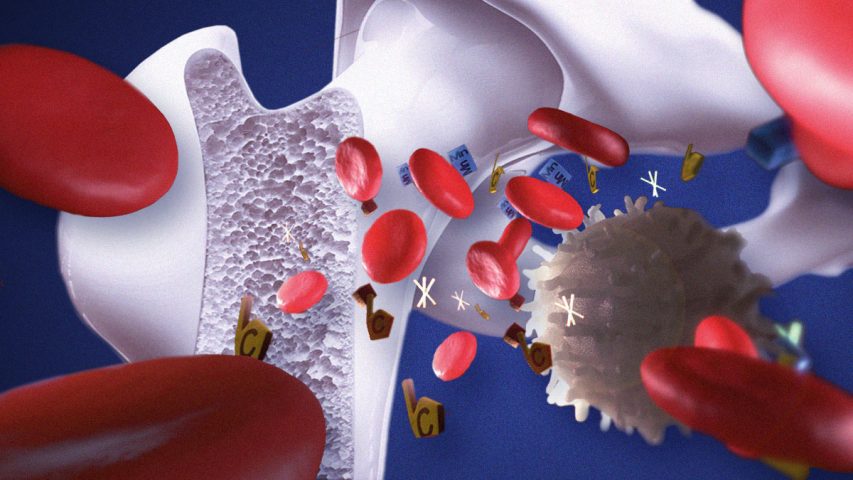
In healthy adults, bone tissue is continuously being broken down and replaced. Over a period of between 7 to 10 years, this results in the body’s entire skeleton being completely renewed. As people grow older however, and especially in women after the menopause, bone tissue begins to be broken down more quickly than it can be replaced. This weakens the bones and, as their density becomes lower, makes them more prone to fractures. In osteoporosis the bones become increasingly brittle and fragile, with the result that they can fracture very easily.
Until suffering their first fracture, osteoporosis patients often suffer no symptoms. When symptoms do occur, however, they can include problems such as back pain, a loss of height, and a stooped posture.
To diagnose osteoporosis, your GP will most likely perform a test known as a bone density scan. This measures how many grams of calcium and other minerals are contained in a square centimeter of bone. In general, the higher the mineral content, the higher is the density of the bone. The denser your bones are, the less likely they are to fracture.
Risk factors for osteoporosis
Known risk factors for osteoporosis include the following:
| » Your sex: Women are significantly more likely to develop osteoporosis than men. |
| » Your age: The risk of osteoporosis increases with age. |
| » Certain medical conditions: The risk of osteoporosis is higher in people who suffer from Celiac disease, inflammatory bowel disease, kidney or liver disease, cancer, rheumatoid arthritis, and certain other health problems. |
| » A lack of physical activity: Numerous studies show that weight-bearing exercise improves bone mineral density. |
| » Excessive consumption of alcohol: Chronic alcohol abuse is a known risk factor for osteoporosis. |
| » Smoking: Research shows that cigarette smoking lowers bone density and significantly increases the risk of developing osteoporosis. Smoking is so dangerous that even inhaling secondhand smoke is associated with a risk of osteoporosis. |
| » The use of certain pharmaceutical drugs: A number of prescription drugs are known to place patients at an increased risk of developing osteoporosis. For example, around 30-50% of patients on long-term corticosteroid therapy will experience osteoporotic fractures. Long-term use of proton pump inhibitors can significantly increase the risk of suffering osteoporosis-related bone fractures. |
Conventional treatment of osteoporosis
Unfortunately, the pharmaceutical drugs prescribed for osteoporosis can cause severe side effects and do more harm than good.
The bisphosphonate class of drugs that are commonly used to treat osteoporosis are particularly dangerous and, rather than strengthening bones, have been found to make them weaker. In a study carried out by scientists at Imperial College in London, use of these medications was associated with the development of ‘microcracks’ in bone. Significantly, the bones of patients taking bisphosphonate drugs had a larger number of such cracks and less mechanical strength than those who weren’t.
Other research has found that treatment with so-called Selective Estrogen Receptor Modulators (SERMs), a class of estrogen-boosting drugs used to treat osteoporosis in postmenopausal women, increases the risk of developing cancer. Osteoporosis patients who take the hormone calcitonin also have an increased risk of cancer.
The Cellular Medicine approach to osteoporosis
Dr. Rath’s Cellular Medicine approach addresses the root cause of osteoporosis by supplying optimum amounts of specific micronutrients that are needed to build and maintain healthy bones. While many people mistakenly believe that vitamin D and calcium are the only micronutrients needed for healthy bones, this overlooks the fact that the framework of the bone on which calcium and other minerals are deposited is made of a protein – collagen. Without healthy collagen, bone cannot form or function properly. Healthy bone formation therefore depends not only on having sufficient amounts of calcium and vitamin D, but more importantly on a proper supply of vitamin C, the amino acids lysine and proline, and other collagen-supporting micronutrients.
In addition to his Basic Cellular Health Recommendations, Dr. Rath recommends that patients suffering from osteoporosis or at risk of developing the condition should take the following micronutrients in higher dosages:
| VITAMIN C – Vitamin C plays a vital role in promoting the formation of collagen for normal functioning of the bones. Research shows that serum vitamin C levels are lower in patients with osteoporotic fractures. Supplemental vitamin C should be taken as part of a synergistic formula that includes the amino acids LYSINE and PROLINE, which similarly play essential roles in the formation of collagen. |
| VITAMIN A – Vitamin A is essential for the growth of bone and plays important roles in the normal functioning of osteoblasts (cells that build new bone) and osteoclasts, (cells that break down bone so that it can be repaired and remodeled). |
| VITAMIN E – Research shows that low intakes and low serum concentrations of vitamin E are associated with an increased rate of bone fracture in elderly women and men. |
| VITAMIN D & VITAMIN K – Research shows that vitamins D and K play a synergistic role in maintaining bone health. |
| FOLIC ACID – Research shows that elderly people with low levels of the B vitamin folic acid (folate) have an increased risk of suffering osteoporotic fractures. |
| CALCIUM – Research shows that an increased calcium intake and a high dietary calcium/phosphorus ratio has favorable effects on bone mass. When taken in combination with vitamin D3, supplemental calcium has been shown to reduce the risk of hip fractures and other nonvertebral fractures. |
| MAGNESIUM – Magnesium plays important roles in the maintenance of bone health. It is involved in calcium metabolism, the synthesis of vitamin D, and the integrity of skeletal bone-crystal formation. Research shows that magnesium supplementation can prevent fractures and significantly increase bone density. |
| POTASSIUM – Research shows a positive association between potassium intake and bone density, thus suggesting that supplemental potassium can play a role in osteoporosis prevention. |
| ZINC – Research shows that, compared to healthy people, patients with osteoporosis have lower serum levels of zinc. A randomized double-blind, placebo-controlled clinical trial carried out in Iran has shown that postmenopausal women with osteoporosis may benefit from zinc supplementation. |
| MANGANESE – Manganese influences the formation of osteoblasts and osteoclasts. This makes it essential for normal bone growth and development. |
| BORON – Boron has a powerful effect on calcium metabolism. Research suggests that in postmenopausal women, supplementing a low-boron diet with boron induces changes consistent with the prevention of calcium loss and bone demineralization. |
| IODINE – An essential element for bone mineralization, research shows that urinary iodine levels are significantly lower in women with postmenopausal osteoporosis. |
| SILICA – A growing body of the scientific literature recognizes that silica plays an essential role in bone formation and maintenance. Supplementation with silica has been shown to increase bone mineral density and improve bone strength. Silica can therefore play an important role in the natural prevention and treatment of osteoporosis. |
If you would like further information on preventing or controlling osteoporosis using natural approaches, please feel free to contact us.



